One of the perilous illnesses that can be characterized by the separation of the retina, a delicate tissue layer found at the rear of the eye, is retinal detachment. Failure to promptly resolve this illness that affects vital eye parts may result in permanent blindness that cannot be treated.
It is commonly recognized as an ocular condition that requires prompt surgical attention. This particular problem is frequently detected in individuals who have a family history of the condition or a notable degree of close-range vision impairment.
It is commonly recognized as an ocular condition that requires prompt surgical attention. This particular problem is frequently detected in individuals who have a family history of the condition or a notable degree of close-range vision impairment.
Signs To Be Aware Of
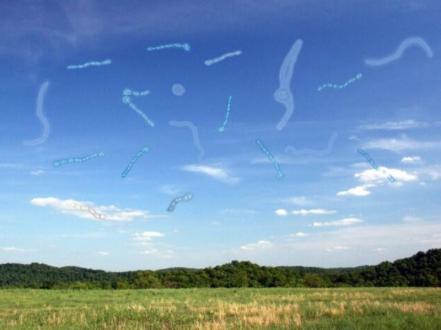
Retinal detachment doesn’t provoke any painful sensations, so this is an extremely unusual sign. Light flashes in one or both eyes and the presence of floaters—small particles that seem to be floating through one's field of vision—are two visual signs that may indicate potential problems. On top of that, those who are impacted can see a lowering curtain or shadow across their field of view or have hazy sight. In such cases, it is critical to get medical help right away.
Caring Tactics
The main goal of surgical treatments used to treat the condition is to restore the tissue's adherence to the posterior ocular wall and fix any retinal tears or fissures that may have formed. Depending on the severity, urgency, or other eye diseases, a vitrectomy, pneumatic retinopexy, or scleral buckling operations may be performed.
Although there exists a range of efficacious care tactics, early recognition continues to be critical for successful treatment. Consistent eye exams are pegged as a critical measure in mitigating risks, particularly for individuals aged 40 and above or those who are in the category of higher risks. It is a severe condition, but it is possible to anticipate a substantial restoration of vision with prompt medical aid.
Although there exists a range of efficacious care tactics, early recognition continues to be critical for successful treatment. Consistent eye exams are pegged as a critical measure in mitigating risks, particularly for individuals aged 40 and above or those who are in the category of higher risks. It is a severe condition, but it is possible to anticipate a substantial restoration of vision with prompt medical aid.