Usually, severe irritation of the iris and ciliary body—the eye's major layers—is triggered by anterior uveitis. Depending on the main location of damage, iritis or iridocyclitis might have catastrophic repercussions if left unaddressed.
Manifestations of the issue
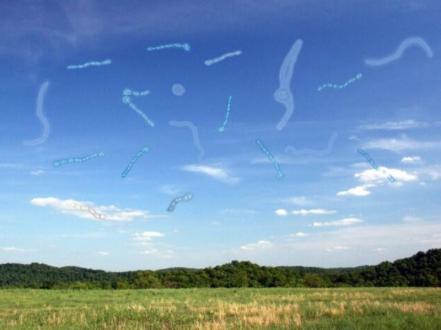
Timely detection and therapy require an in-depth comprehension of the signs and etiology. Rapid development of redness, floating objects, aversion to light, pain, and distorted vision is possible. The etiology is frequently obscure. However, potential contributors include infections, trauma, autoimmune disorders, and toxins. Acute uveitis is distinguished by symptoms of rapid eye irritation.
Risk factors and variables that cause severe outcomes
Macular edema, band keratopathy, and cataracts can all develop from unmanaged anterior uveitis. It is brought on by systems such as sarcoidosis or ankylosing spondylitis.
Techniques of care
Caring success requires prompt initiation based on the cause and severity. Using corticosteroids or incorporating eye drops or pills are frequently used as first-line treatments. Extra medications like cycloplegic might be used. Medications that are specifically designed for infections are also prescribed.
Implications and monitoring requirements
The consequences of prolonged corticosteroid use must be monitored; therefore, observation is critical. Ongoing monitoring is pivotal for determining the efficacy of a caring tactic and identifying adverse effects. In the event of vision impairment, cataract surgery might be required.
Managing pre-existing uveitis
In order to prevent potentially hazardous effects on vision, symptoms must be promptly detected and treated. This potentially hazardous ocular condition necessitates continuous collaboration and interaction between treatment providers and patients. Preventing a recurrence of the issue requires that patients undergo routine eye examinations.