Comprising the sclera of the eye and the retina, the uvea is a critical component of the intricate ocular architecture. This intermediate layer guarantees the best performance by controlling light entering the eye and nourishing its tissues. Its upkeep is quite important since compromised uveal tracts can affect general ocular health, bring unwanted discomfort, and lead to vision problems.
What is the Uvea?
Comprising the iris and ciliary body, the uveal layer is the middle one of the eye. These elements taken together protect eye health and aid in maintaining clear vision. The iris controls the light when it enters the eye, therefore adjusting the pupil's size to suit varying light levels. The ciliary body helps focus the lens for clear vision and produces the fluid that maintains intraocular pressure and feeds the eye. There is also the choroid of the eye. It can be affected too. The choroid is responsible for supplying oxygen and nutrients to the retina, therefore maintaining its general vitality and function. These components taken together form a sophisticated process necessary for maintaining clear and intermediate vision as well as for ensuring the health of ocular tissues.
The Uveal Tract: Structure and Function
The uveal tract stresses the connection of the iris, ciliary body, and choroid vital for the function of the eye. It modulates the light entering the retina, adjusts the lens to focus, and provides the nutrients required for the retina to operate as it should. This tract gives structural support and resistance against environmental pressures when working in concert with the sclera. The uvea skillfully balances retinal feeding, lens accommodation, and light regulation to maintain general visual acuity and health.
Common Disorders of the Uvea
Diseases affecting the uveal layer can damage its function, leading to a range of ocular disorders. Among such conditions is uvea inflammation, sometimes known as uveitis. Usually presenting as redness, pain, or blurred vision, trauma, autoimmune reactions, or infections could all cause this condition; untreated, it can have significant effects.
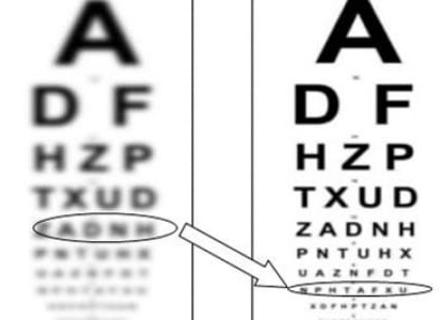
Another common condition that affects the choroid and is frequently associated with two systemic diseases, autoimmune diseases or hypertension, is choroidopathy. Such diseases can influence retinal nutrition and induce rising vision loss. Early identification and treatment of these issues determines most importantly the state of eye health. Regular professional visits or even an eye test at home can help identify any problems, therefore ensuring quick intervention.
How to Maintain a Healthy Uvea
The long-term viability of the visual system depends on the uvea being properly maintained. Any anomalies in the uveal system can be found mostly by regular eye tests before they become major causes of trouble. Wearing premium sunglasses helps shield the eyes from the damaging consequences of UV radiation, therefore preventing damage. Eating a well-balanced diet high in omega-3 fatty acids and antioxidants helps the eye, including the uveal layer, be generally healthy. Taking breaks and cutting the time spent in front of screens helps one avoid eye strain and preserve the finest possible eyesight.
One Last Remark
Apart from vision, the uveal layer is a basic part of the eye that helps preserve general ocular health. Knowing its makeup and purposes helps one appreciate its part in the visual system. The long-term health of an individual's eyes will be determined by the formation of good habits, giving routine eye care for the quick resolution of any possible problems a top priority, so preserving both their eyesight and quality of life.