Xanthelasma is a flat, benign, yellowish, slightly elevated plaque that is most often localized on the upper eyelid at the inner corner of the eye. It is a local accumulation of cholesterol by skin cells.
Xanthelasma Causes
The exact cause of xanthelasma is not known. Approximately half of the patients have fat metabolism disorders. Xanthelasma can be a sign of the following diseases:
- familial hyperlipidemia type IIa (familial hypercholesterolemia), type IIb (familial combined hyperlipidemia), and type IV (familial hypertriglyceridemia);
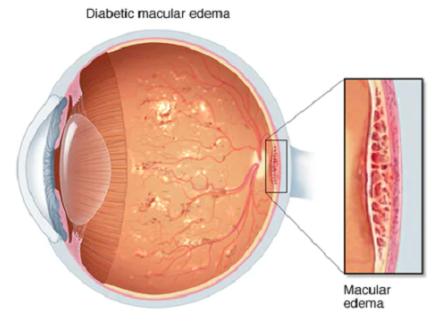
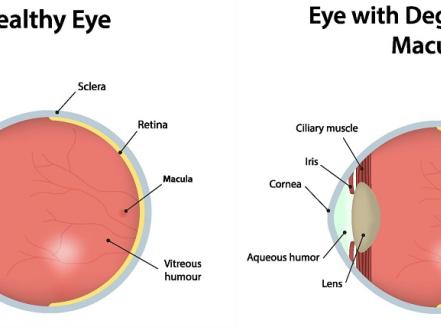
- diabetes mellitus;
- hypothyroidism;
- obesity;
- systemic atherosclerosis;
- primary biliary cirrhosis;
- pancreatitis.
Xanthelasma can also occur in patients who have previously had contact dermatitis or generalized cutaneous dermatoses.
Xanthelasma risk factors
Risk factors for xanthelasma include:
- female;
- age from 35 to 55 years old;
- smoking;
- obesity;
- high blood lipid levels;
- hypertension;
- diabetes mellitus.
Symptoms of Xanthelasma
Xanthelasma is a yellowish plaque on the upper eyelid, painless, soft, slightly protruding above the skin, single or multiple, growing slowly and not accompanied by discomfort. However, patients may experience psychological discomfort and desire to get rid of this cosmetic defect. Rarely, ptosis (drooping) of the eyelid can occur.
Xanthelasma can also be a manifestation of a generalized disease — xanthomatosis. In this case, yellow plaques or nodules can occur on various skin areas (face, neck, buttocks, knee, and elbow joints) and even on the mucous membrane of the mouth. They are called xanthomas and are also associated with cholesterol deposition.
Xanthelasma Diagnosis
Diagnosis includes visual examination, slit-lamp examination, and diascopy. It is also necessary to consult an endocrinologist and dermatologist. A blood lipid panel (indicators of fat metabolism: lipoprotein and cholesterol fractions) is mandatory, and the risk of atherosclerosis and cardiovascular pathology is necessarily calculated.
Xanthelasma Treatment
Xanthelasma treatment should be complex. The patient should correct the diet and physical activity, depending on the identified fat metabolism disorder or other metabolic abnormalities. In addition, drug therapy (statins, fibrates, nicotinic acid) is prescribed to lower cholesterol levels, normalize glucose levels (in diabetes mellitus) or thyroid hormones (in the case of the pathology of this organ).
Xanthelasma can be removed only by surgery. For its removal, it is used:
- surgical excision (in the case of large xanthelasma and the presence of ptosis);
- cryoablation;
- laser removal (using Q-switched, Nd:YAG, Er:YAG or carbon laser);
- fractional radiofrequency destruction.
Complications after surgery:
- Relapse of xanthelasma (without normalization of blood lipid levels, the risk of xanthelasma recurrence is very high).
- Scar formation (with a tendency to form keloid scars).
- Skin pigmentation.
- Ectropion (eyelid eversion).
Xanthelasma Prevention
To prevent the development of xanthelasma, you need to monitor your weight, adhere to proper nutrition (with low consumption of animal fats), and also eliminate bad habits.
Prognosis
As noted earlier, xanthelasma tends to recur. The prognosis depends on effective treatment of the underlying disease and adherence to a healthy lifestyle.
Xanthelasma may be an early sign of atherosclerosis (accumulation of lipids in the vascular walls), so dietary recommendations and lowering blood lipids also reduce the risk of stroke and heart attack.
Expert's Opinion