Demodicosis is a parasitic infection caused by an opportunistic pathogenic mite of the genus Demodex. This mite is a normal inhabitant of human hair follicles and sebaceous glands. But when its population increases, it can cause skin inflammation. In addition, the Demodex mite can affect eyelashes and eyelids, and then the disease is called ocular demodicosis.
Ocular Demodicosis Causes
Two types of Demodex mites parasitize on human skin — Demodex folliculorum (lives in the hair follicles) and Demodex brevis (lives in the sebaceous, meibomian, and Zeiss glands). Mites are most common in the facial area due to the abundance of sebum required for their development.
Their relationship with humans is commensalism (the mite gains benefits and the person does not suffer). But under certain conditions (lowered immunity, poor hygiene, etc.) the number of ticks increases, damaging the human body and causing chronic inflammation. Because of their non-specific clinical picture, Demodex mites often cause blepharitis, conjunctivitis, chalazion, episcleritis, trichiasis, and marginal keratitis.
Ocular Demodicosis Risk factors
- an increase in age (Demodex is acquired during the first feeding of a child (because of its presence on the skin of the nipples) and its prevalence only increases with age (the mite is present in 84% of people aged 60 years and in 100% of the population over 70 years old);
- low level of hygiene;
- weakening of the immune system;
- hormonal disorders;
- chronic stress;
- contact lens wear;
- liver and gastrointestinal (GI) diseases;
- work associated with caring for the elderly.
Symptoms of Ocular Demodicosis
Symptoms caused by Demodex mite parasitization include:
- itching;
- burning;
- foreign body sensation;
- сrusts/cylindrical dandruff and loss of eyelashes;
- redness of the eyelids;
- tearing;
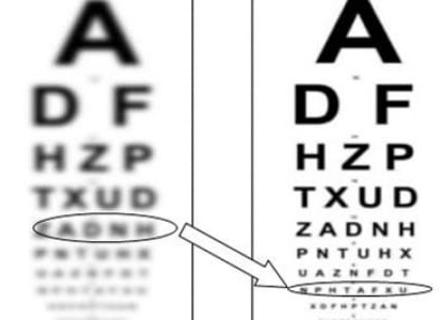
- blurred vision;
- discomfort/irritation.
Often these patients have seborrheic or atopic dermatitis, rosacea. Also, due to abnormal functioning of the meibomian glands, patients with demodicosis develop dry eye disease.
Demodicosis Diagnosis
The slit-lamp examination is used for diagnosis, which allows visualizing both the mites and the sign of their parasitism – cylindrical scales at the root of the eyelashes. Eyelashes are also examined under a microscope. To do this, 4 eyelashes on each eyelid are epilated and placed on a glass slide for examination with a microscope.
However, the presence of mites is not always the basis for a diagnosis of demodicosis. It is considered normal to have 1-2 mites on 16 eyelashes. An increase in their number over 4 and the presence of clinical signs indicate the presence of ocular demodicosis.
Ocular Demodicosis Treatment
The treatment of ocular demodicosis is always complex. It is necessary to improve hygiene and regularly sanitize everything that touches the face (pillow, towel, glasses, etc). It is also recommended not to use cosmetics for the entire course of treatment.
Tea tree oil (TTO) has been proven effective in the fight against Demodex mites due to the presence of terpinen-4-ol (T4O) in its composition. There are specially formulated shampoos, scrubs, lotions, gels, and wipes for daily use with 20%-50% tea tree oil. The doctor can also perform the first procedure at the appointment, using a higher concentration of TTO than the one the patient will use at home.
Among antidemodex medications, the most effective are Ivermectin, Permethrin, Metronidazole, Ornidazole, Erythromycin, and Clindamycin. They are prescribed for severe inflammation and insufficient effectiveness of local medications. In addition, artificial tears are prescribed for the treatment of dry eye disease.
A treatment period of at least 6 weeks is recommended to cover two life cycles of the Demodex mite.
It is also necessary to treat liver and gastrointestinal diseases, and foci of chronic infection.
Prognosis
Relapses of ocular demodicosis occur in 10% of cases. Usually, they are associated with an incomplete treatment course, lack of personal hygiene, and the presence of concomitant pathology