Diabetic macular edema is a chronic disease that develops as a result of the body's inability to produce enough of the hormone insulin or the inability to use it effectively. Patients suffering from diabetes mellitus are at high risk of developing many complications that affect various organ systems.
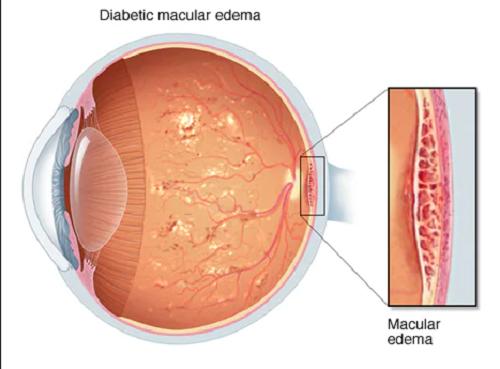
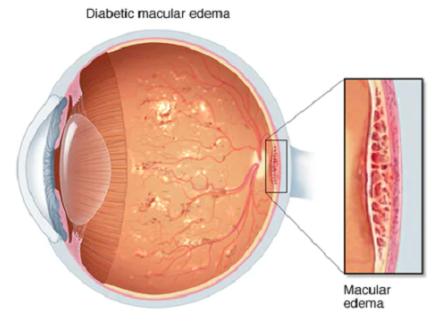
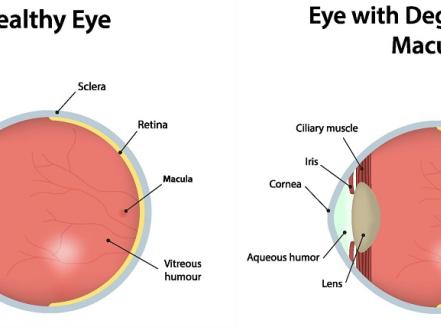
One of these is diabetic retinopathy, which can cause severe vision loss. As a result of fluid seepage from the vessels into the retina, macular edema develops — Diabetic macular edema ICD 10 (DME) — deforming tissue and causing visual impairment. If untreated, it can lead to complete loss of central vision.
Diagnostics of the Diabetic macular edema
To define diabetic macular edema of the eye, first, the history and conduct of an examination of the fundus is studied carefully. Then the patient can be directed to optical coherence tomography — a highly informative method for examining the retina, with which it is possible to identify even the slightest changes in its structure.
Diagnosis of DME is based on both general ophthalmological examination data and specialized instrumental methods. The diagnostic standard for DME is retinal fluorescence angiography and diabetic macular edema OCT.
Symptoms of diabetic macular edema
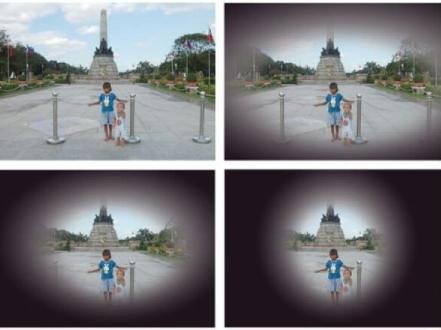
Macular edema in diabetic retinopathy may present early with few symptoms. Moreover, it is also characterized as a painless condition. Remember to tell your doctor if you notice the following symptoms in your vision:
- Blurry vision;
- Doubling;
- Floating ‘flies’ in the eyes.
If you have diabetes, your eyes should be checked regularly. In some cases, macular edema can appear quickly, as in the case of retinal venous thrombosis.
The causes of diabetic macular edema:
- increasing the permeability of the internal hemato-ophthalmic barrier in the endothelial cells of the retinal vessels;
- decrease in oncotic pressure of blood plasma in kidney disease;
- an increase in hydrostatic pressure in blood vessels with arterial hypertension;
- deterioration of venous outflow with venous thrombosis;
- dysfunction of the retinal pigment epithelium (RPE);
- adhesions in the vitreous body, which can stretch the retina and increase vascular permeability.
Types of diabetic macular edema
It is a well known fact that DME develops in about one in three people with diabetes for 20 years or more. Macular edema is divided into several types:
- focal;
- diffuse macular edema;
- cystic macular edema of the retina;
- ischemic maculopathy.
In some cases, diabetic macular edema occurs after cataract removal, it is also called Irwin-Gass syndrome. Post-thrombotic macular edema is also one of the main causes of decreased central vision in patients with retinal vein occlusion. For the treatment of macular edema in such patients, intravitreal drugs are used that belong to the group of VEGF factor inhibitors and corticosteroids.
Diabetic macular edema treatment
For a long time, laser coagulation of the retina was the only way of how to prevent blindness in patients with diabetes mellitus. There are two types of treatments commonly used to treat diabetic macular edema, both of which are aimed at preserving the patient's vision and preventing further vision loss:
- Laser treatment for local DMO — using laser light, leaking blood vessels are closed, preventing more fluid from entering the macula. The patient should be re-examined three months after treatment to ensure that the DME is responding to treatment.
- Diffuse DMO laser treatment — lattice laser is used to narrow the dilated blood vessels. As with the treatment of local DMO, the patient should be reevaluated three months after surgery to ensure that DME is responding to treatment.
For diabetic macular edema, the main treatment is to normalize blood sugar levels. To do this, you need to contact an endocrinologist.
The most significant risk factors for the development and progression of DR are considered: insufficient glycemic control, arterial hypertension, nephropathy, hypertriglyceridemia, pregnancy, hypercholesterolemia, genetic factors.