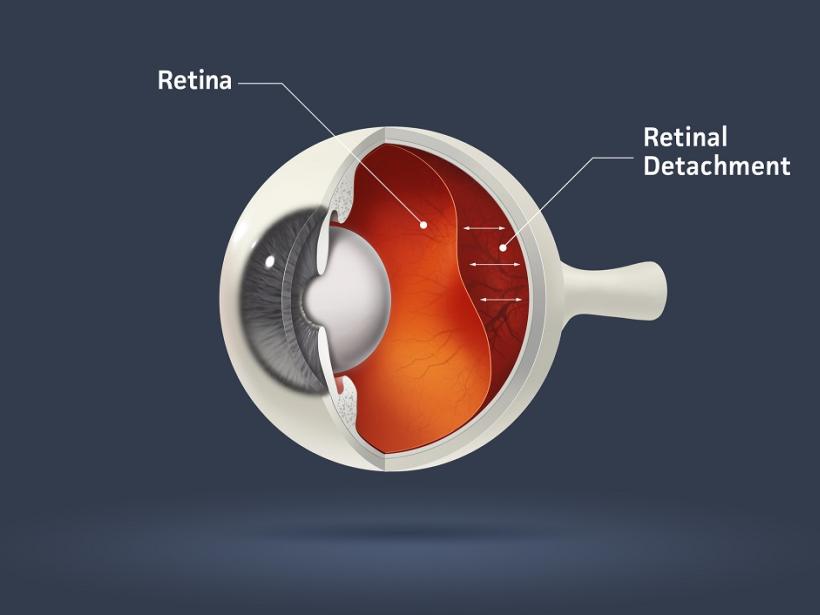
Retinal detachment is a pathological condition in which the retina separates from the choroid (the vascular layer of the eye).
The retina is the part of the eye that is directly responsible for the perception of light (thanks to rods and cones), it’s processing, and the transmission of information to form a visual image. The retina is located at the back of the eye and is a very thin structure, which adheres tightly to the choroid, which provides its constant nutrition. In some cases, this close contact is disrupted, which, without immediate surgical treatment, leads to the death of the retinal cells and irreversible loss of vision.
Causes and types of retinal detachment
There are several types of retinal detachments depending on the cause:
- Rhegmatogenous (from the Greek rhegma — tear) retinal detachment is caused by a retinal rupture through which fluid from the vitreous body seeps under the retina. This is the most frequent type of detachment. The rupture is caused by thinning and dystrophy of the retina.
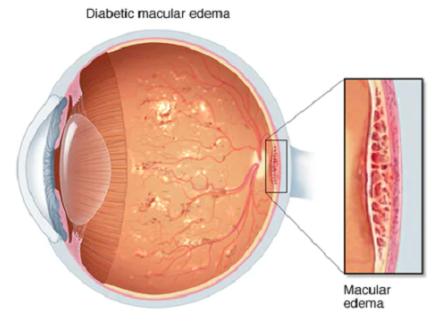
- Tractional detachment is associated with tension (traction), due to the formation of fibrinous bands or new pathological vessels in the vitreous body (for example, in diabetic retinopathy).
- Traumatic detachment is associated with eye trauma or surgery. It can also occur several years after the trauma/surgery.
- Secondary detachment is associated with the occurrence of tumors, inflammatory diseases of the choroid and retina, hemorrhage and thrombosis, retinopathy of prematurity, etc.
- Exudative (serous) detachment occurs when the fluid starts to accumulate under the retina, as a result of some pathology, while there is no rupture of the retina.
- Mixed — for example, a tractional-rhegmatogenous detachment (the tear is formed against the background of traction of the vitreous body).
At-risk are patients with:
- Moderate to high myopia.
- Diabetes mellitus.
- A history of eye trauma or eye surgery.
- Circulatory disorders.
- Cases of retinal detachment in close relatives.
- Peripheral vitreoretinal degeneration.
- Work associated with constant physical stress and heavy lifting.
Retinal detachment symptoms
Retinal detachment is a painless process. It can develop in just a few seconds, or it can last for years. The main symptoms to suspect this pathology are:
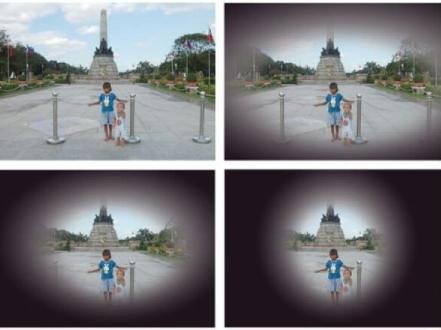
- Short-term flashes of bright light (lightning, sparks);
- Floating objects-shadows in the field of view (multiple "eye floaters");
- Blurred vision, and gray veil with progression;
- Narrowing of the field of vision, loss of some parts of the field of view;
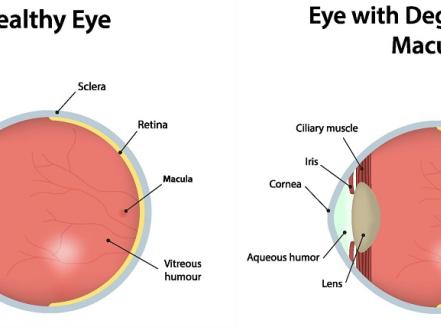
- With the detachment of the central part of the retina (macula), there is a significant decrease in visual acuity, distortion of objects, or their complete loss from the field of view.
Sometimes patients note that in the morning the symptoms decrease or disappear altogether. This is because in the horizontal position, the retina returns to its place and the fluid is absorbed more intensively. But still, during the day, the symptoms reappear.
Some types of detachment (traction or exudative) can be completely asymptomatic, so it is very important to visit an ophthalmologist regularly.
How is retinal detachment diagnosed?
The complex of diagnostic procedures includes:
- Visual acuity measurement;
- Perimetry (examination of the visual fields);
- Tonometry (determination of intraocular pressure);
- Special electrophysiological examination to determine the viability of nerve cells of the retina and optic nerve;
- B-mode ultrasound of the eye, to determine the size of the detached retina and the condition of the vitreous body;
- Examination of the fundus with a dilated pupil (ophthalmoscopy) to determine the localization of retinal tears and their number;
- Optical coherence tomography (to detect the smallest retinal tears).
Consequences of retinal detachment
If surgery is not performed in time, retinal detachment can lead to the following complications:
- Blindness.
- Persistent loss of a part of the field of vision or a veil.
- Distortion of objects and a significant decrease in visual acuity.
Treatment
It is important to understand that no pills, drops, or injections will help put the retina back in its original place and fix it. The only treatment for retinal detachment is surgery. The earlier it is performed, the better the chances of successful restoration of vision.
- Methods for the surgical treatment of retinal detachment include:
- Coagulation (sealing with diathermy (laser)) — the tissue around the retina is scarred, which prevents fluid from seeping under the retina.
- Pneumatic retinopexy — the defect is sclerosed by freezing or using a laser. Then, sterile air is injected into the vitreous cavity, which brings the retina back into its place.
- Vitrectomy (the vitreous body is removed and replaced with gas, saline solution, or silicone; after a certain period, the gas is dissolved and filled with its moisture, while the silicone is removed surgically);
- Local scleral buckle (a small silicone band (scleral buckle) is sewn on the sclera so that it is drawn inward and together with the choroid comes close to the retina) is made for partial detachment;
- Circular scleral buckle is used in case of a complete retinal detachment;
- Retinal ballooning (a balloon catheter is temporarily sutured to the sclera in the projection area of the detachment; the balloon is inflated and results in the same effect as the scleral buckle).
The method of treatment is chosen individually, taking into account the characteristics of the rupture (localization, quantity, degree of detachment, how much time has passed since it appeared). Several stages of surgical treatment may be required.
Complications of surgical treatment:
- Cataract formation (loss of transparency of the lens of the eye);
- Glaucoma (increased pressure in the eye);
- Infectious inflammation (uveitis);
- Hemorrhage (bleeding) into the cavity of the vitreous body;
- Vision loss.
Prevention
It is recommended to visit an ophthalmologist once a year for preventive purposes, even if you are not at risk. Patients with moderate and high myopia should not lift very heavy objects, beware of atmospheric pressure fluctuations and avoid traumatic sports. Blood pressure and blood sugar levels should also be monitored. Your ophthalmologist may recommend vitamin complexes and drugs that improve the nutrition of the retina and strengthen it.
In the presence of retinal thinning and a high risk of tearing with subsequent detachment, prophylactic peripheral 360◦ laser photocoagulation is a modern and highly effective preventive method. It is a painless and safe method that allows using a laser to create point adhesions between the retina and the choroid, thereby significantly reducing the risk of retinal detachment.