Vitrectomy ("vitreum" means vitreous body, "ectomy" means removal) is a surgery to remove the vitreous body (the transparent gel that fills the eye cavity) followed by its replacement with saline, sterile air, or silicone oil.
Indications for vitrectomy
Vitrectomy is necessary if the vitreous body is infected, inflamed, filled with blood or tissue fragments (vitreous body destruction or "eye floaters"). Also, this type of surgery can help the ophthalmologist treat some retinal pathology.
Eye diseases that may require a vitrectomy to treat:
- Diabetic retinopathy.
- Proliferative vitreoretinopathy.
- Bleeding inside the eye (intraocular hemorrhage or hemophthalmia).
- Destruction of the vitreous body
- Retinal tears and detachment.
- Epiretinal membranes.
- Injury or trauma to the eye.
- Macular holes, macular degeneration with neovascularization.
- Complications after cataract surgery.
- Complications associated with uveitis.
Diagnostics
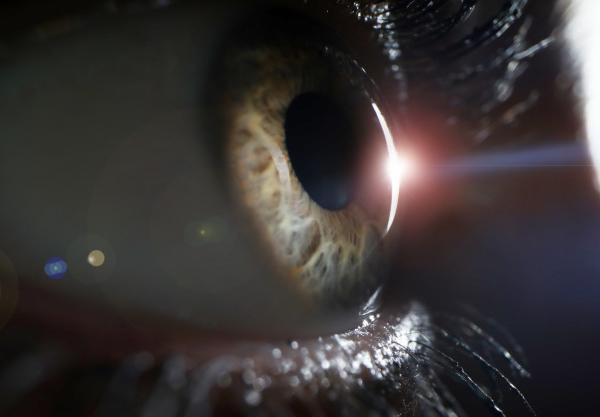
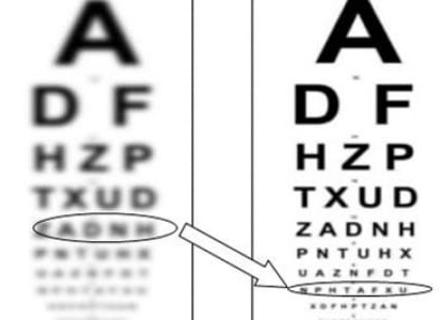
Examination methods include measurement of visual acuity, eye biometry, and dilated pupil examination. Ultrasound is most commonly used to determine the condition of the vitreous body.
Additional diagnostic methods may also be needed, such as:
- Optical coherence tomography (OCT) provides a layer-by-layer image of the retina to identify its pathology.
- Fluorescence angiography visualizes retinal vascular lesions using intravenous contrast.
How is a vitrectomy performed?
Vitrectomy is an outpatient surgery. It is performed under local anesthesia (sometimes under general anesthesia) and usually takes 40-120 minutes, depending on the severity of the pathology. This procedure can also be combined with other interventions (e.g. cataract removal).
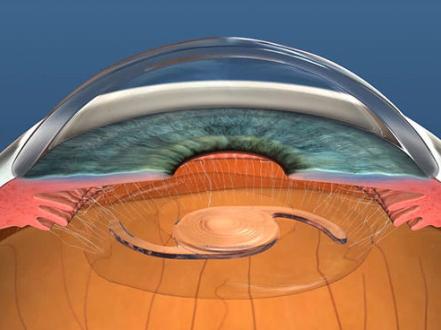
During the surgery, the ophthalmic surgeon makes three small incisions (half a millimeter each) in the white part of the eye (the sclera), and then ultra-thin surgical instruments are inserted through them. A fiber optic light guide is used to illuminate the retina. A cannula is used to irrigate and maintain intraocular pressure, and a vitrector is used to cut and remove the vitreous body. After the removal of the vitreous fluid, retinal treatment (laser cauterization, restoration of integrity, etc.) is performed if necessary. Further, gas is injected into the cavity of the posterior chamber. In more severe cases and for more secure fixation of the retina, silicone oil is injected. After a few months, the gas is self-absorbed into the tissue, and the cavity is filled with aqueous humor produced by the ciliary body. And the silicone will need to be surgically removed after a few months.
Postoperative period
- The bandage that covers the eye is taken off the next day.
- The patient uses antibiotic eye drops for one week and anti-inflammatory drops for several weeks.
- The patient may experience mild discomfort or a foreign body sensation when blinking.
- The patient may have transient redness of the eyes or swelling of the eyelids.
- Immediately after surgery, the patient returns to usual daily activities without significant restrictions. But during the first month, it is recommended to avoid sudden head movements, heavy physical activity, and driving.
- If the eye cavity is filled with gas, it is not recommended to climb to a high altitude and to fly by plane until the gas has completely dissolved, because this can provoke a sharp increase in intraocular pressure. Also, a specific head position (face down or on a determined side while sleeping) is necessary for several weeks.
- Due to the dilated pupil of the operated eye, there may be an increased sensitivity to bright sunlight in the first two weeks. Therefore, it is recommended to wear sunglasses.
- The injection of gas or silicone oil temporarily impairs vision, which improves after a few weeks or months.
Complications and risks
In 90% of cases, the operation is successful and does not lead to complications.
Very rarely, such complications may occur:
- Postoperative bleeding into the eye cavity.
- Retinal detachment.
- Increased intraocular pressure.
- Formation and rapid progression of cataract.
- Infectious inflammation of the eye (endophthalmitis).
- Problems with eye movement after surgery.
- Changes in refractive error.
Also, there is a risk that the surgery may not successfully correct the original problem. In this case, a second vitrectomy may be necessary