Selective laser trabeculoplasty (SLT) is a gentle and non-invasive laser therapy used to treat glaucoma.
SLT is used:
- as primary therapy for open-angle glaucoma;
- in combination with eye drops that lower intraocular pressure (IOP) if they are not effective;
- after unsuccessful glaucoma surgery or argon laser trabeculoplasty (ALT).
Why is it called selective?
The SLT laser has minimal absorption of thermal energy. The energy of the SLT laser is absorbed only by individual cells that contain melanin pigment. Therefore, this type of laser is sometimes referred to as a «cold laser». That’s why the procedure is painless and doesn't cause scarring, unlike ALT, in which there is significant thermal damage to the tissues of the eye.
What is the mechanism of selective laser trabeculoplasty?
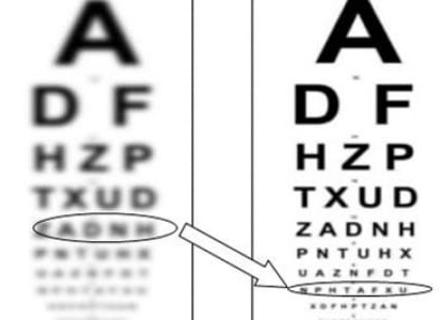
SLT uses laser pulses to stimulate the natural healing mechanism to lower intraocular pressure. Using a special wavelength (532 nm) and energy, the laser affects only the pigment cells of the eye. This improves the outflow of intraocular fluid, which in turn lowers the intraocular pressure.
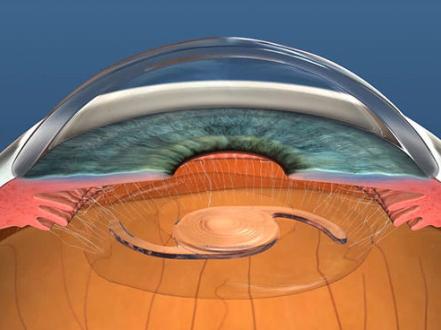
To maintain a normal IOP, the intraocular fluid must constantly drain through a special formation at the corner of the anterior chamber, which is called the trabecular meshwork. During SLT, an ophthalmologist uses a laser to correct this anatomical formation.
Indications for SLT
- Primary open-angle, pseudoexfoliative or pigmentary glaucoma.
- Glaucoma drug intolerance/difficulty in using glaucoma medications.
- Inadequate IOP lowering with drug therapy for glaucoma (combination therapy).
- History of treatment failure with ALT (argon laser trabeculoplasty).
What are the contraindications for SLT laser?
- Angle-closure glaucoma;
- uveitic glaucoma;
- post-traumatic glaucoma with angle recession;
- congenital glaucoma;
- juvenile glaucoma;
- angle dysgenesis;
- neovascular glaucoma.
How is SLT performed?
SLT is an outpatient procedure that takes only a few minutes. You will sit in an examination chair and your doctor will use a specially designed microscope (slit lamp) to visualize the structures of your eye. This slit lamp has a built-in laser that is used to perform SLT. Before the procedure, the doctor will put some anesthetic drops in your eye. The ophthalmologist will place a contact lens on your eye for better imaging. After focusing the beam, the doctor forms small holes in the trabecular meshwork to help improve the outflow of intraocular fluid.
Selective laser trabeculoplasty is a painless and bloodless procedure. However, the lens that is used to focus the laser may irritate your eye. You will also see a green flash of laser light that may blind you for several minutes after the procedure.
SLT side effects
Adverse reactions and side effects after SLT are very rare. These include:
- Inflammation (iritis, uveitis);
- temporary elevation of intraocular pressure (in 5% of patients);
- eye pain or inflammation of the conjunctiva (the transparent membrane covering the white part of the eye);
- hyphema (blood in the anterior chamber of the eye);
- corneal edema;
- abrasion of the corneal epithelium;
- scarring in the angle of the anterior chamber;
- temporary refractive shift to hyperopia.
How often do you need to have SLT?
Unlike ALT, SLT can be performed multiple times. Intraocular pressure lowers significantly about three days after the procedure (by 20-30% in 75-85% of patients). However, results may take 1 to 3 months to appear. One SLT session leads to a stable decrease in intraocular pressure over several years. Another procedure may be necessary depending on your condition.
Rehabilitation period
After the procedure, anti-inflammatory eye drops are prescribed and the patient returns to his or her daily routine. You may also drive a car. In case of insufficient IOP reduction, you may need additional use of eye drops to lower your IOP